My Microscopic Fellow Travelers To China
A strange new microbe appeared in my gut during a trip to Beijing.
During my Mexico travel experiment, I tested only three times: before, during, and after. Did I miss anything by not testing daily? On a recent trip to Beijing, I decided to find out.
International travel always presents major challenges to the microbiome. Besides the significant differences in food, you are surrounded by different people, different climate, and different germs. A trip to China involves a 12 hour plane flight too, exposing the body to a long period of lowered air pressure, tight quarters with people and recycled air, and of course the jet lag that accompanies a fifteen hour time shift. With all of that, it would not be surprising to see a significant shift in my microbiome.
Here’s an overall heat plot of my gut, day-to-day before and after the trip:
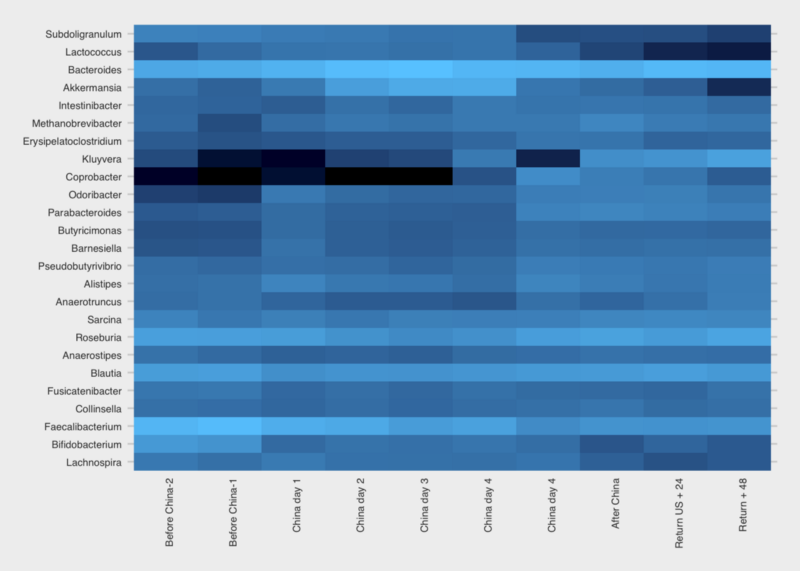
Figure 1: Gut samples before/during/after a trip to Beijing from the US. Darker colors are low abundance, lighter colors are higher abundance
I wasn’t surprised to see the rise in Kluyvera, a genus that on the 16S test can include sometimes-pathogenic species like E. coli or Shigella. These microbes can go up and down regularly, sometimes for no apparent reason at all, but often due to a significant change in environment, like on a trip where you’re exposed to many new microbes.
But the obvious standout is the genus Coprobacter, which soared beginning a few days after arrival and settled back after my return. I looked in my other samples over the long term and find that it is strongly associated with my China trip.

Figure 2: Changes in gut microbiome abundance of Coprobacter over time. Area shaded in red is the period while traveling from the U.S. to China. Daily samples for the rest of the time period shown have zero or minimal abundance.
Among my years of daily sampling it appears to have bloomed only once — this trip — after which it settled back to its quiet little self. The very first time I noticed any at all was early in the year, coincidentally (?) after I began drinking kefir. But even then, the amounts were tiny (under 0.01%) and often zero — until this trip.
When I looked at the hundreds of other samples people have sent me, I could find Coprobacter in just a few, and then only at relatively small levels (under 0.4%), less than a tenth of what I found on my biggest day (4.9%). The big 4000+ person Zhernakova study found many people who have some, but generally in trivial amounts. I couldn’t see any obvious patterns in any of the samples: some were from heavy travelers including some who had been to China, some not; some were from healthy people, some not. I found small amounts in a few skin samples (including my son, in a sample taken shortly after my return), but always in small amounts and with no clear patterns.
The natural question to ask about this microbe is what does it do? Unfortunately, as in so many of these cases, even Dr. Google can’t tell me much besides a few passing references in hundreds of top academic papers. It doesn’t seem to be a well-studied microbe. I know that it’s a member of the Bacteroidetes phylum, a “rod-shaped, gram-positive, obligate anaerobe”, and my particular species appears to be Coprobacter fastidiosus.
The Russian scientists who first isolated it (in 2013) found that, when cultured on glucose, it generates propionic, acetic, and succinic acids. Look up those acids and you can invent creative stories that might explain why it appeared on my trip to China (smelly? maybe the food! retinal modulation? maybe from the smog!). But I’ve been around the microbiome block enough to know that you can explain just about anything if you try hard enough and you don’t care about proving it scientifically.

Figure 3: Source: Shkoporov et al (2003) A scanning electron microscope image of my species of Coprobacter. OM = Outer Membrane, PS = Periplasmic Space, Asterisks denote unrecognized electron-dense patches in some cells
Other Microbes
Travel is often good for Proteobacteria, another large family of microbes that changed on this trip. Whenever I see high levels, in myself or others, I usually find that the body is undergoing some kind of challenge — often as a result of exposure to something unhealthy, like a sick person or bad food, and sometimes accompanied by symptoms like an upset stomach or fever. Are the symptoms a result of the higher levels of Proteobacteria or a cause? Maybe this phylum contains plain old pathogens, which would explain the rise in abundance, or maybe — and I’m speculating — it rises as a natural defense to protect us ?

Figure 4: Gut Proteobacteria abundances rose during a period of heavy travel. Note: zero abundances are days with no samples available.
Whatever the reason, my levels clearly rose (Figure 4). Shortly after returning home, I was on another plane, for a week in the Midwest. All that travel appears to have kept my Proteobacteria levels high. (Unfortunately I’m missing a few samples during that period, but I think you can see the trends). I was never ill during my trip — at least not with symptoms I could feel — but my previous bouts of illness almost always coincide with a bump in Proteobacteria, so who knows.
How about diversity? Did that change?

Figure 5: Shannon diversity of gut samples during a week-long trip to Beijing.
Answer: maybe. Diversity is an imprecise measure, and mine seems to bounce up and down for no apparent reason anyway. It’s not surprising that exposure to an all-new environment would bring new microbes too, as in the case of Coprobacter. Incidentally, I continued traveling throughout the US the week or two after returning from China — lots of airplanes — so it wouldn’t be hard to understand an uptick in microbial diversity.
Conclusion
International travel to a very different place, like China, is associated with noticable changes to my microbiome. There is at least one gut microbe, Coprobacter, whose bloom seems highly correlated to this particular trip. I also tested my skin, mouth, and nose microbes during the trip and found some interesting surprises there too, but I’ll write that up in a future post.
Like my other experiments with kombucha, Soylent, and a low-carb high fat diet, I’m accumulating evidence that it’s possible to manipulate the microbes inside me — my microbiome. Although we generally think of our genes as unchangeable, these microbes contain far more genes than we get from our parents, and I’m excited about the possibility that I might be able to change my genetics, perhaps through simple changes to diet or geography. If future research shows that Coprobacter is good for me, I now know an easy way to get some!
Meanwhile, if you’d like to test your own microbiome, you can take 15% off the price if you use the offer code ‘PERSONALSCIENCE’ on a uBiome Explorer gut kit. And be sure to send me the results when you get them, so we can see if you have Coprobacter too.
References
Shkoporov, A. N., E. V. Khokhlova, A. V. Chaplin, L. I. Kafarskaia, A. A. Nikolin, V. Y. Polyakov, V. A. Shcherbakova, Z. A. Chernaia, and B. A. Efimov. 2013. “Coprobacter Fastidiosus Gen. Nov., Sp. Nov., a Novel Member of the Family Porphyromonadaceae Isolated from Infant Faeces.” INTERNATIONAL JOURNAL OF SYSTEMATIC AND EVOLUTIONARY MICROBIOLOGY 63 (Pt 11): 4181–8. doi:10.1099/ijs.0.052126–0.
Zhernakova, A., A. Kurilshikov, M. J. Bonder, E. F. Tigchelaar, M. Schirmer, T. Vatanen, Z. Mujagic, et al. 2016. “Population-Based Metagenomics Analysis Reveals Markers for Gut Microbiome Composition and Diversity.” Science 352 (6285): 565–69. doi:10.1126/science.aad3369.
Originally published at richardsprague.com on April 2, 2018.


